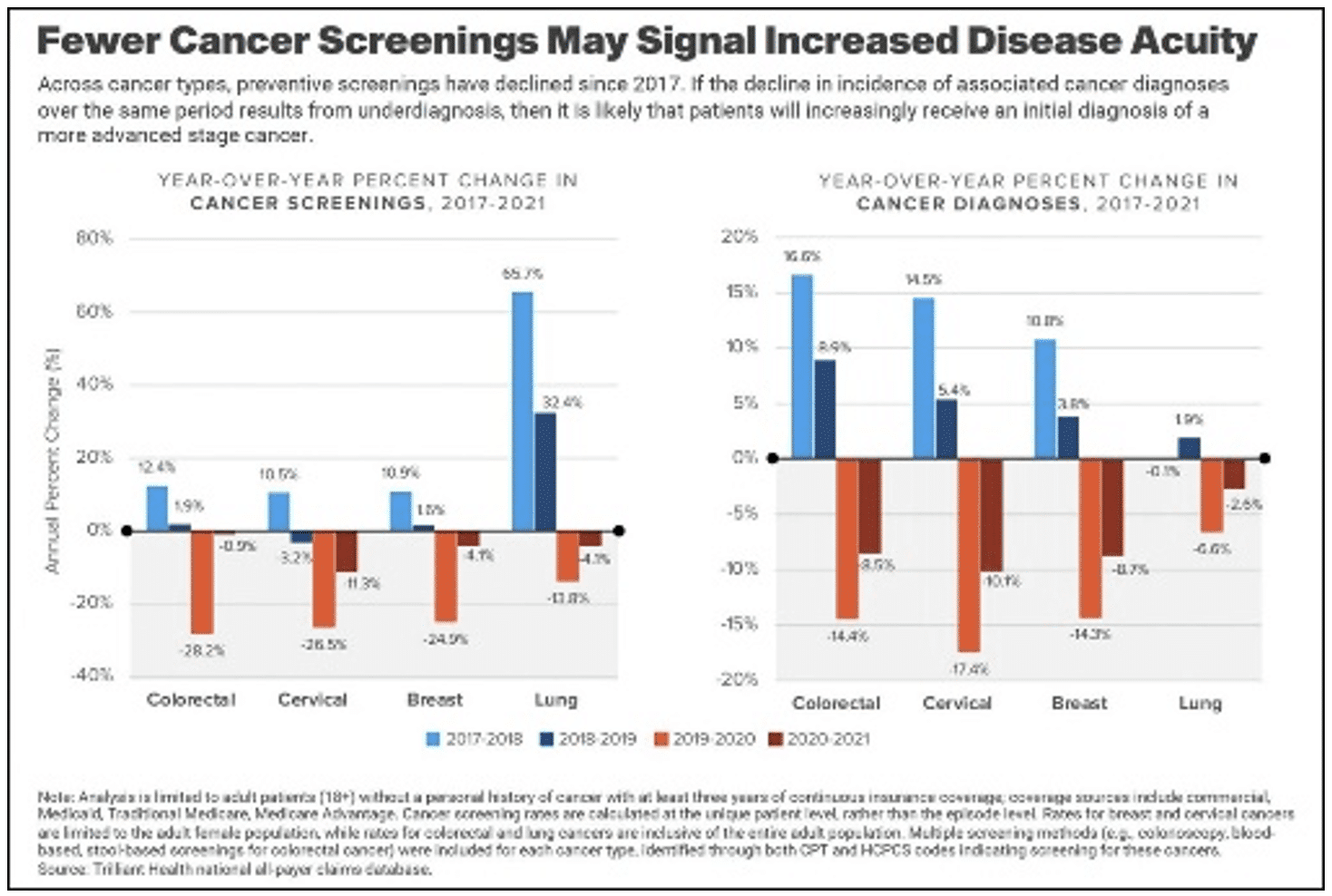
Breast cancer screenings declined by 25% between 2019 and 2020, and the trajectory continued downward at 4% decline annually. Unsurprisingly, diagnoses dropped, on average, 11.5% between 2019 and 2021. Declines were also observed in other cancers, with up to double-digit decreases since 2020.1
Early detection is more vital but overcoming an outdated “one-size-fits-all” requires adapting new technologies. Every woman’s breast cancer journey is her own. Fortunately, one of today’s most rapidly developing technologies is making the detection and treatment of breast cancer more effective and personal.
“Artificial intelligence (AI) continues to revolutionize various spheres of our lives,” reports the Cureus Journal of Medical Science. “Faster, more accurate results are some of the benefits of AI…in breast cancer screening.” The diminished effectiveness of treatment in late-stage breast cancer makes AI-driven diagnosis and treatment crucial to improved prognosis and reduced mortality.2
Human intelligence takes existing knowledge, processes new information and elevates learnings to adapt, identify patterns and assign meaning. AI uses these same abilities to learn and improve blindingly fast, converting images of tissue specimens on glass slides to digital images and storing histologic information. That data warehouse enables comparison and analysis of other images to detect variations, evaluate disease, progression2 and enable personalized treatment.
The journal Radiology reports that researchers have utilized AI to predict risk.3
“There’s much more information in a mammogram than just the four categories of breast density,” says study lead author Adam Yala, PhD candidate at the Massachusetts Institute of Technology (MIT). “By using the deep learning model, we learn subtle cues that are indicative of future cancer.”3
The researchers compared three risk assessment approaches: traditional risk factors; mammogram-based deep learning; and a hybrid of the two. They accessed almost 90,000 mammograms from approximately 40,000 women to test the deep learning model, obtaining outcomes from a regional tumor registry and improving risk detection. Comparing the hybrid model against breast density indicated that patients with non-dense breasts and model-assessed high-risk had almost four times the rate of cancer of patients with dense breasts and model-assessed low risk, and those advantages held across subgroups of women. Researchers continue to track AI’s performance and communicate risk to women and their physicians.3
Using more than 25,000 digital screening mammograms from almost 6,400 women, researchers at the University of Hawaii Cancer Center trained a deep learning model to review mammograms for increased cancer risk. It underperformed in assessing risk for interval cancer risk but outperformed clinical factors in screening-detected cancer risk.4
“AI provides a better risk estimate for screening-detected cancer than other forms of assessment,” says UH Cancer Center Researcher John Shepherd. “It helped us [by] classifying women into low risk or high risk of screening-detected breast cancer. By ranking mammograms in terms of the probability of seeing cancer in the image, AI is going to be a powerful…tool [in categorizing] mammograms.”4
The team intends to replicate the study in women typically underrepresented in breast cancer research, Native Hawaiians and Pacific Islanders, then move beyond cancer risk to look at different grades of breast cancer, from least to most aggressive.
Dr. Susan Holley, a radiologist with UNC Health in Chapel Hill, ran a study that utilized approximately 214,000 exams of over 61,000 patients, interpreted by 39 radiologists at 50 different clinics. Density assessments were categorized as constant, bidirectional, ascending, and descending. She incorporated all four categories to compare the resulting density patterns to show that the AI model produced significantly more constant assessments than the radiologists. Variations in comparison data lead to the same results.
“Moreover, these results held for several subgroups in our dataset, including patients interpreted only by breast fellowship trained radiologists, in women older than 55—presumed to be post menopausal and thus with less hormonal variability—and even in cases interpreted by the same radiologist,” says Holley.
Forward-thinking providers and innovative tech partners, including Onsite Women’s Health, will offer breast cancer screening and diagnostic services with clinical expertise and proprietary protocols in a compassionate concierge approach. Statistical models incorporating elements of a patient’s health history and AI-driven assessment will allow patients and physicians to assess risk and manage treatment which, along with screening compliance, reduces cancer mortality by 50%.5 Patients will benefit from a comprehensive, convenient, accurate and profoundly personal offering.
Healthcare organizations like Onsite Women’s Health genuinely committed to offering personalized breast care will utilize every tool, including AI, to provide a “one-stop-shop” delivery model for women compliant with recommendations about mammograms. Only then can truly meaningful data, based on centralized radiological and genetic expertise, drive mammography and breast health services that provide peace of mind and a “win/win” for patients and providers, alike.
[1] Undiagnosed cancer could be the next health crisis — and we aren’t ready
[2] Artificial Intelligence in Breast Cancer Screening and Diagnosis
[3] Novel Artificial Intelligence Method Predicts Future Risk of Breast Cancer

